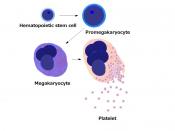
It is important to take into consideration the compatibility of platelets when they are transfused into a patients. Unlike RBC transfusions, there are really no ABO compatible platelet transfusions. Platelet transfusions should be classified as either ABO identical or non identical. Subsequently, whenever a problem arise with platelets transfusion it is either going to be a minor ABO incompatibility, major incompatibility or Rh incompatibility.
Minor incompatibility occurs when the donor plasma contains ABO antibodies that are not compatible with the recipients platelets. This kind of transfusion causes a positive DAT to occur, sometimes causing hemolytic reaction. For example the study in the article showed that none of the 82% of patients who received non identical platelets had any significant hemolysis. The determinant factor for hemolysis depends on the concentration the amount of antibody transfused as well as the blood type of the donor. With O being highest in concentration and B lowest in concentration.
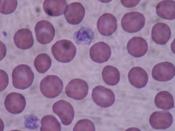
Major Incompatibility occurs when red cells that have a surface antigen is being transfused to patient that has the antibody to the antigen. For example when B platelets are transfused to a group 0 recipient. This results in platelets refractoriness, thereby reducing the platelet count, and sometimes platelets death.
Rh antigens are not expressed on platelets, although survival of transfused platelets is not dependent on RhD incompatibility. Residual red cells in platelets senistize RhD negative patients receiving RhD positive platelet. This is a problem for pregnant women if incompatibility arise, because it leads to hemolytic disease of new born. Therefore, it is important to inject anti-D immune globin to the mother if Rh negative platelets are not available for transfusion in order to prevent the disease.
The most obvious adverse effect of transfusing ABO nonidentical platelets is hemolysis. The risk of an ABO hemolytic reaction is rare after a single transfusion of ABO nonidentical platelets, but increases significantly when large volumes are transfused over a relatively short time periodHemolysis is unlikely after a single ABO incompatible unit for two reasons. First, transfused plasma (500 mL) is diluted almost 10 fold in the patient's intravascular blood volume (5000 mL). Second, and perhaps most importantly, transfused anti-A and anti-B antibodies are rapidly neutralized by binding to circulating soluble A and B antigens as well as tissue A and B antigens.
Transfusion of platelets containing large volumes of ABO incompatible plasma saturates soluble and tissue ABO antigen sites and permits binding of excess anti-A and/or anti-B to red blood cells. When this happens, patients develop a positive direct antiglobulin test (DAT) and possibly hemolysis.
Chronically transfused patients with hematologic disease who are transfused with nonidentical ABO platelets have lower post-transfusion platelet counts, require almost twice as many platelet transfusions, and develop platelet refractoriness earlier than patients receiving ABO identical platelet transfusionsTransfusion of group A or B platelets to group O recipients results in post-transfusion platelet increments that Transfusion of group O platelets to group A or B recipients results in even lower post-transfusion platelet increments, suggesting that incompatible plasma is an even more important risk factorare 20% less than those obtained with ABO identical platelet transfusionshttp://www.clinlabnavigator.com/transfusion/platelettransfusion.html