Microbiology T, Th
Superbug
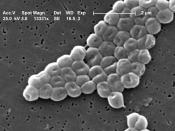
Acinetobacter
A new study reports a surge in drug-resistant strains of a dangerous type of bacteria in US hospitals: Acinetobacter strikes patients in Intensive Care Units (ICUs) and others and often causes severe pneumonias or bloodstream infection, some of which are now resistant to imipenem, an antibiotic that is reserved for last-line treatment. As well as affecting ICU and other patients, Acinetobacter infections are arising in soldiers returning from the war in Iraq.
Where did Acinetobacter originate from?
Acinetobacter baumannii is a non-fermentive, aerobic, opportunistic, gram-negative coccobacillary rod. Morphological findings vary according to the phase of cell growth and exposure to antimicrobial agents. Widely distributed in soil and water, A baumannii grows at various temperatures and pH environments and uses a vast variety of substrates for growth. The indiscriminate nature of this organism and its recent acquisition of MDR intensify its emergence and significance in healthcare environments.
There are at least 25 different types of Acinetobacter. These bacteria are widely found in nature, mostly in water and soil.
The organisms have also been isolated from the skin, throat, and various other sites in healthy people. Acinetobacter baumanni is the type that is most often associated with hospital-acquired infections but does not typically colonize healthy people outside of hospital settings.
How do you get it?
According to the US Centers for Disease Control and Prevention (CDC), Acinetobacter bacteria are common in soil and water, and can also be found on the skin of healthy people, especially those working in the healthcare profession.
This is very scary stuff since I work as a C.N.A. The bacteria spread through person-to-person contact, contact with contaminated surfaces, or exposure in the environment. While Acinetobacter poses little risk to healthy people, those with weakened immune systems, chronic lung disease, or diabetes may be more susceptible to infections, as are very ill hospitalized patients on ventilators, those with a prolonged stay, or those with open wounds. How is it treated?
Most types of Acinetobacter are easily treated with common antibiotics and with other supportive care. Other types of Acinetobacter, and especially those acquired in hospitals, can be resistant to many commonly prescribed antibiotics and require special treatments. Health care providers identify treatment options for each infection on an individual basis.
How to prevent it:
Isolation and infection control procedures such as hand washing and wearing of gowns and gloves by those who have contact with infected patients are used to prevent transmission to others in our medical treatment facilities. Military medical staffs know that the numbers of Acinetobacter infections increase in battlefield situations because of the types of traumatic injuries service- members suffer. Because of this, they are paying increased attention to infection control procedures and have been told to watch carefully for early signs of infection.
In closing here are some fast facts on Acinetobacter:
Acinetobacter bacteria are common in the environment but are rarely a medical threat to healthy, uninjured persons.
Acinetobacter can be acquired by person-to-person contact, through contact with contaminated surfaces, or as a result of wounds contaminated with dirt and debris.
Some types of Acinetobacter are resistant to antibiotics and can be severe and especially difficult to treat if they result in bloodstream infections.
Persons most at risk of difficult-to-treat Acinetobacter infections are those who are very ill, have traumatic wounds, and are treated in intensive care units.
Frequent hand washing and disinfection of medical treatment facilities are the best ways to avoid spreading Acinetobacter.
Works Cited:
http://science.journalfeeds.com/general-science/plos-one/multidrug-resistant-acinetobacter-baumannii-risk-factors-for-appearance-of-imipenem-resistant-strains-on-patients-formerly-with-susceptible-strains/20100401/
http://www.nature.com/jp/journal/v24/n8/full/7211133a.html
http://www.up.ac.za/dspace/handle/2263/3925
�PAGE �